CLINICAL
specialty contact lenses
Get in the Cone Zone: Part 1
Follow these six fitting tips for keratoconus patients.
ROXANNA T. POTTER, O.D., F.A.A.O., SYLVANIA, OHIO
With so many contact lens options now available for keratoconus patients, it’s almost as difficult to decide where to start as it is to find the perfect fit. From standard corneal GP, intra-limbal, scleral, soft and soft toric lenses to piggyback and hybrid designs, an ideal lens for virtually every corneal shape exists.
Here, in part one of this two-part series, I provide six fitting tips that can help ensure successful contact lens wear in keratoconic patients, regardless of lens choice. Part two, written by Melissa Barnett, O.D., F.A.A.O., discusses the aforementioned contact lens designs in more detail, so you can choose the optimal lens relative to each patient.
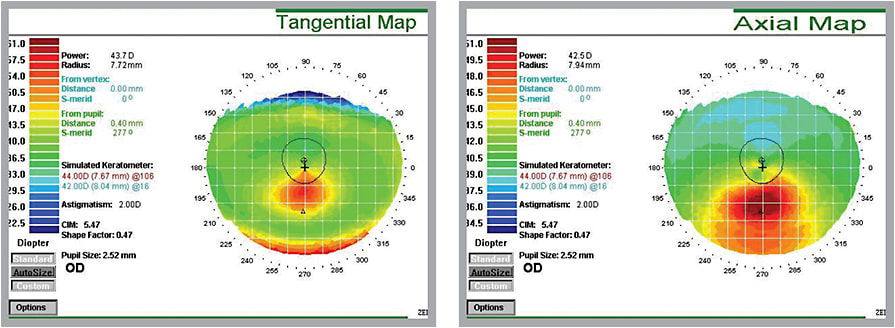
Notice how the cone size is more accurately shown in the tangential display (left) vs. the axial display in corneal topography.
1 Be mindful of ocular surface disease.
Keratoconic patients are often dependent on their lenses and are, therefore, unable to limit their wear time despite marked discomfort. While the jury on the link between eye rubbing and keratoconus progression is still out, it nevertheless makes sense to try to alleviate any potential ocular surface disease (OSD) that may result in symptoms, such as dryness and irritation, that elicit aggressive eye rubbing by the patient. A careful assessment of symptoms, thorough patient questioning and diagnostic investigation followed by diligent OSD management improves the keratoconic patient’s contact lens-wearing experience in ways that no contact lens design, no matter how great, can achieve alone. (See “OSD: A Practice Builder,” page 40.)
2 Think sagittal depth.
Sagittal depth principles apply to all keratoconic fits. Comprehending sagittal depth facilitates problem solving when a patient has an unusual corneal size or shape, allows for increased understanding of many new and emerging scleral lens designs and helps reduce fitting time for all keratoconic lenses because it influences individual contact lens parameters, such as base curve and diameter selection. As a result, it’s time to stop depending on individual contact lens parameters.
3 Analyze more than one topographical display.
The axial display of a corneal topography is, arguably, the most intuitive to most practitioners when evaluating irregular corneas for contact lenses. This is because it reveals a sort of average curvature across the entire measured cornea with relative steep and flat areas shown to represent the overall cornea shape. For this reason, it is tempting to quickly look at an axial map of a keratoconic patient to choose the initial diagnostic lens. That said, details that can aid in fitting irregular corneas, such as corneal elevation, could easily be lost in this view. Therefore, you should also reference the elevation and tangential maps prior to selecting a diagnostic lens. The elevation map delineates small areas of corneal elevation or depression. This map can help localize the cone’s apex, for example, to aid in the differentiation between an inferior, oval cone and pellucid marginal degeneration. The tangential map is less representative of overall cornea shape and more accurate in actual curvature at each point; this is of particular use in the periphery of irregular corneas.
Analyzing the specific elevation and curvature of the more irregular areas of the cornea helps predict problems with lens centration, bearing and pooling on steep or flat areas and minimizes the number of diagnostic lenses required during the fitting. This allows for a more efficient fitting, and patients appreciate both the speed and accuracy of the fit as well. (Most specialty lens lab consultants can receive e-mail or faxed copies of the topographies to assist you during the fit.)
4 Invest in anterior segment imaging.
Anterior segment imaging can save both you and the patient time and money in irregular corneal contact lens fitting. Specifically, it allows you to access saved photos or video and review diagnostic lens fit characteristics, such as those outlined above. This is particularly helpful when troubleshooting ongoing fit issues, such as persistent edge lift or decentration. Media files can even be shared with specialty lens lab consultants to assist in difficult cases.
5 Use the same contact lens solutions.
Using the same solution during the fitting process that you recommend the patient use at home helps prevent unexpected sensitivity issues and patient confusion. This applies to all keratoconic lenses, both soft and GP, and is particularly important when fitting keratoconic patients in scleral lenses.
Many practitioners use standard GP lens solutions for insertion, removal and training of scleral lenses. These solutions have well-known benefits for scleral lens GP materials: They provide excellent lens wetting and initial comfort, and the increased viscosity of many of these solutions allows for a thick, cushion-like effect that patients enjoy. Due to preservative toxicity of these standard GP lens solutions, however, patients are told to buy preservative-free saline for lens filling and wear at home. The difference between the volume of solution retained under the scleral lens and resultant sagittal depth can be quite different vs. the standard GP lens solutions, and both initial fit appearance and lens-settling amount changes based on the solution used to fill the scleral lens.
Until a high-viscosity, preservative-free solution for both fitting analysis and at home becomes commercially available (and financially feasible), stock up on preservative-free saline or viscous preservative-free artificial tears in the office to emulate conditions the patient will have at home.
6 Encourage regular lens replacement.
Keratoconic patients should be encouraged to replace their GP lenses at least annually, if not more often as they are at additional risk of corneal scarring due to apical bearing and corneal compression brought on by warped or damaged lenses. An example of a patient conversation about this: “Mr. Smith, it is important you replace these lenses every year. As these lenses age, they can become warped, chipped and scratched, which can eventually cause eye damage.”
Also, explain to patients that regular lens replacement ensures smooth adaptation to new lenses rather than the difficulty often encountered when parting with an old pair. This prevents the frustration that occurs (for both the patient and you) when newly ordered replacement lenses demonstrate worse vision or comfort vs. the patient’s previous lenses, despite having the same ordered parameters.
A fitting end
Regardless of which lens designs you select for your keratoconic patients, the six aforementioned tips not only facilitate the fitting process, but also provide greater ease in switching between the various options available. OM

| Dr. Potter is in private practice in Sylvania, Ohio. She has designed and participated in numerous research projects and has given lectures to both students and optometrists on eye-related topics. E-mail her at Rpotter@personaleyecare.com, or send comments to optometricmanagement@gmail.com. |



