As the COVID-19 pandemic has wreaked havoc, causing fear, illness, a financial crisis and loss of life, the significantly higher incidence of serious complications and death among diabetic patients has served as a stark reminder of the long-standing diabetes pandemic itself1 (see a “History of Diabetes” at end of this article). Here, we’ll discuss the statistics of diabetes and, specifically, how we as doctors of optometry can “flatten the curve” of diabetes.
THE STATISTICS
Today’s diabetes statistics are well known, but still astounding:
- Diabetes is the seventh leading cause of death in the United States (although it’s likely significantly higher, due to its impact on other conditions, such as cardiovascular disease).2
- More than 34 million Americans have diabetes (~11% of the population), with 1 in 5 unaware of their diagnosis.2
- More than 88 million Americans have prediabetes, with >84% of them not knowing it.2
- There were about 1.5 million new cases of diabetes in 2018 in U.S. adults age 18 or older.3
- It is predicted that 1 in 3 adults will have diabetes by 2050.4
- Diabetes is the leading cause of vision impairment worldwide in the 20 to 74 age group.4
- Diabetes is the fifth leading cause of blindness worldwide.5
- An estimated 20% to 40% of patients with Type 2 diabetes already have retinopathy at their initial diabetes diagnosis.6,7
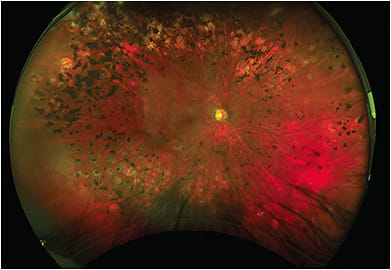
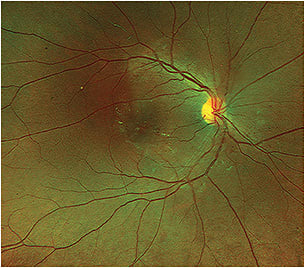
While we appropriately focus on diabetic retinopathy (DR) because of its potentially sight-threatening complications, diabetes also is associated with increased incidence of papillopathy, glaucoma (all forms), ocular surface disease (including dry eye disease), cataracts and keratopathy.
These mind-boggling statistics underscore the vital role doctors of optometry play in the care of diabetic patients, both in the anterior and posterior segment of the eye, and their overall systemic health.

HOW TO MAKE A DIFFERENCE
It all starts with education and communication. We can:
- Keep our eyes open. Just this year, the FDA approved a second standalone, artificial intelligence (AI)-based screening system to automatically analyze retinal photographs for signs of diabetes, without a doctor of any kind being involved. While AI-based systems can be a useful adjunct to doctor-driven exams, we must be proactive in identifying the pathology of diabetic eye disease in our offices, corresponding with other members of the patient’s health care team, such as their primary care provider, and reporting our findings to the patient’s insurer.
- Provide patient education. As Timothy Petito, O.D., has pointed out in his work on behalf of the profession through various volunteer roles with the American Optometric Association, it’s not simply a finding of retinopathy that yields better overall diabetic health outcomes, it’s the conversations we have with those patients that drive home the message and produce positive change. AI-based retinopathy screening platforms, which don’t involve patient-doctor interaction, can’t effectively replicate that, especially since we are often the entry point to the health care system as patients seek relief from presbyopia, and then later develop age-related eye diseases, such as glaucoma and cataracts. In summary, we have a unique opportunity to emphasize to patients the importance of managing their diabetes and other systemic diseases.
Explaining and allowing patients to view the images of their eyes captured in the office (e.g. photos and/or OCT scans when retinopathy is present) can be an extremely powerful driver of compliance, especially when also reminding patients their retinal health is a good indicator of how other organ systems are likely faring with their disease. These simple, brief discussions can have a lasting and significant impact, fostering adherence to both prescribed treatments and follow-up appointments. - Encourage blood sugar control. Taking a few extra seconds to encourage patients reduces their chances of diabetes-related vision loss:
“Mr. Smith, watching what you eat, taking your medications, exercising moderately and keeping your doctors’ appointments are critical to helping control your blood sugar, which significantly reduces your chances of vision loss, as well as other complications from diabetes.”
PROVIDE A GUIDE
Diabetic patients across the country are benefitting from doctors of optometry who actively seek and manage diabetes, creating patient loyalty and receiving referrals from friends, family and other health professionals with whom they collaborate on care. For more advice and guidance on caring for these patients, Dr. Zach McCarty provides an overview of the latest diagnostic tools and strategies aiding in the detection of diabetic eye disease in “Diagnose Diabetic Eye Disease,” p.20; Drs. Mohammad Rafieetary and Jessica Haynes discuss new and emerging diabetic eye disease treatments in “Treat Diabetic Eye Disease,” p.26; and Dr. Peter Cass explains the practice management implications and opportunities that caring for diabetic patients affords in “Dive Into Diabetic Eye Care,” p.30.
As primary eye care physicians, it is incumbent upon all of us to stay abreast of this pandemic disease. There is likely no greater opportunity within our profession to have such a profound impact on patient morbidity and mortality than with diabetes, so let’s seize the opportunity and make a difference! OM
A History of Diabetes
The disease was first described in written manuscripts circa 1500 B.C. in both Egypt and in India, with the term “diabetes” first being used in Greece in 230 B.C. As early as circa 400 A.D., Indian physicians distinguished Type 1 and Type 2 diabetes mellitus as separate conditions. The name “diabetes mellitus” literally means “to pass through honey sweet,” referring to a patient’s urine glucose level. Believe it or not, early on, urine was actually tasted for sweetness to aid in diagnosis (and doctors and lab techs worldwide are forever grateful for the advent of blood glucose analysis). Yet despite its early discovery, naming and classification, there was still no effective treatment for diabetes for over 1500 years.
A century ago, on Oct. 30, 1920, in London, Ontario, a young medical school professor named Frederick Banting was notified at the last minute he would be lecturing on carbohydrate metabolism the following day. As a result, he rushed to the library and furiously researched the topic, of which he knew very little, so he wouldn’t embarrass himself in class. That night, after retiring to bed, he happened to scan the November 1920 edition of the journal Surgery, Gynecology, and Obstetrics, which had just arrived in his mail, and noticed an article about the Islets of Langerhans in the pancreas. Unable to sleep and with his newfound knowledge of carbohydrate metabolism, he formulated an idea, which he scribbled down that night. He would ligate the pancreatic ducts of lab dogs, keeping them alive, and attempt to isolate the secretions from the Islets of Langerhans in hopes they might be used to treat glycosurea. What he, of course, isolated and later purified became the first treatment for diabetes mellitus – insulin. That discovery extended and saved countless lives. What if Banting hadn’t been assigned that lecture, meticulously researched the topic, received that journal that same day, and/or read that particular article? Life for many who have diabetes would’ve been drastically different for who knows how long, as up until that time it was largely a terminal illness
REFERENCES
- Worried about the Coronavirus? Here’s what you should know. American Diabetes Association Website. https://www.diabetes.org/covid-19-faq . Accessed September 9, 2020.
- Diabetes Fast Facts. Centers for Disease Control and Prevention Website. https://www.cdc.gov/diabetes/basics/quick-facts.html . Accessed September 9, 2020.
- U.S. Department of Health and Human Services – Centers for Disease Control and Prevention. National Diabetes Statistics Report 2020: Estimates of Diabetes and Its Burden in the United States. 2020. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.Pdf . Accessed September 9, 2020.
- CDC Newsroom: Press Release. Number of Americans With Diabetes Projected to Double or Triple by 2050. The Centers for Disease Control Website. https://www.cdc.gov/media/pressrel/2010/r101022.html . Accessed September 9, 2020.
- The Importance of Treatment With Good Glucose Control Cannot Be Underestimated. People With Diabetes Can Prevent Vision Loss. The National Eye Institute Website. https://www.nei.nih.gov/sites/default/files/2019-06/diabetes-prevent-vision-loss.pdf Accessed September 9, 2020.
- Harris MI, Klein R, Welborn TA, Knuiman MW. Onset of NIDDM Occurs at Least 4-7 yr Before Clinical Diagnosis. Diabetes Care 1992; 15(7):815-19.
- Kohner EM, Aldington SJ, Stratton IM, et al. United Kingdom Prospective Diabetes Study, 30: Diabetic Retinopathy at diagnosis of non-insulin-dependent diabetes mellitus and associated risk factors. Arch Ophthalmol 1998; 116(3):297-303.
OM COVID-19 Resources
For continually updated resources regarding the coronavirus crisis and optometry, please visit bit.ly/OMcoronavirus .





