Use these three cases to aid you in determining custom lens selection
With the continuous expansion of materials and parameters in “ready-to-wear” soft contact lenses, as well as the availability of advanced technologies in scleral, among other RGP lens designs, when should the optometrist go with a custom soft lens?
Here are three cases to help the OD decide.
CASE 1: THE UNSTABLE ASTIGMAT
Patient: U.A., an active 30-year-old female attorney, originally fit five years ago in a monthly soft astigmatic lens, has since undergone multiple refitting in different brands and modalities, as she has never been truly satisfied with the quality and consistency of the vision provided by her lenses. She reports no lens discomfort, and her latest lenses are soft toric dailies.
Exam Findings: Examination in the lenses reveals perfect orientation in primary gaze, 0.50 mm to 0.75 mm movement with blink and on upgaze, and a 20° blink-induced rotational swing of the lenses, 10° in each direction. Full corneal coverage is observed, but with an inadequate 0.5 mm of scleral overlap. Bilateral keratometry and horizontal visible iris diameter measurements yield keratometry readings of 46.00 D and 12.2 mm OU. Clinical impression of the fit is orientational instability due to insufficient overall lens diameter, resulting in inadequate sagittal depth.
The Solution: Custom monthly soft hioxifilcon toric lenses that have a 7.70 mm base curve and a 14.6 mm diameter.
CASE 2: THE EARLY KERATOCONIC
Patient: MK, a 21-year-old male college student presents for an initial contact lens fitting after failing a pre-LASIK screening due to early keratoconus detection. Recent increased prescription changes, though decreased clarity with each new pair of glasses, prompted an interest in refractive surgery. Additionally, the patient divulges he was told he has rapidly advancing astigmatism.
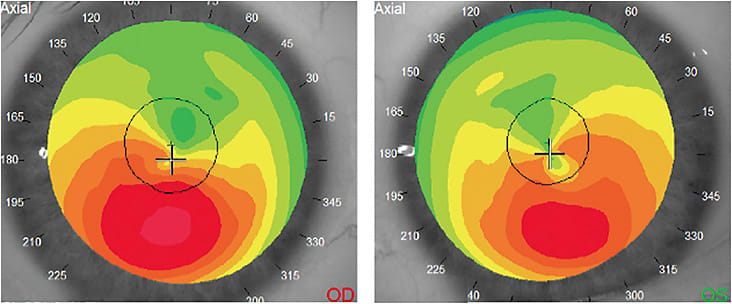
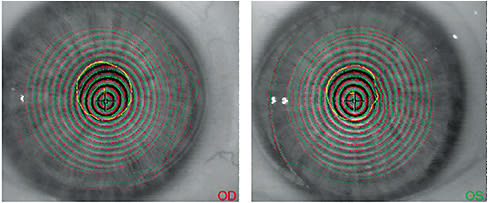
Exam Findings: Topographical and refractive analysis reveals mild-to-moderate keratoconus that has decentered corneal apexes. BCVA is 20/30 OU, with mild “ghosting.” Slit lamp examination shows clear corneas, without significant thinning.
The Solution: A custom soft keratoconic lens to best address the patient’s desire to be able to switch between contact lenses and eyeglasses without “contact lens-induced spectacle blur” and to comfortably manage the early stage of the ectasia. (See Figures 1 and 2.) MK was referred for a corneal collagen crosslinking consultation as well.
CASE 3: THE PRESBYOPIC ENGINEER
Patient: PE, a 45-year-old myopic and astigmatic male mechanical engineer who underwent multiple fitting attempts of a standard design monthly replacement toric multifocal lens presents complaining of unacceptable near vision. He says his goal is optimum far and near vision, and that he is less concerned about intermediate distance vision. Increased add power in standard lens designs has resulted in a reduction of his distance VA.
Exam Findings: PE has smaller than average pupils, measuring 2.8 mm in normal lighting.
The Solution: A custom soft bifocal toric lens that has a bilateral equal add of +1.75 D and central near zones of 1.9 mm and 2.3 mm in his dominant and non-dominant eyes, respectively.
OPPORTUNITIES ABOUND
Custom soft lenses now pro-vide ample opportunity to address the needs of patients whose clinical profile falls outside the range of standard designs.
Also, with the availability of empirical fitting, little-to-no extra chair time is needed for such designs. OM




