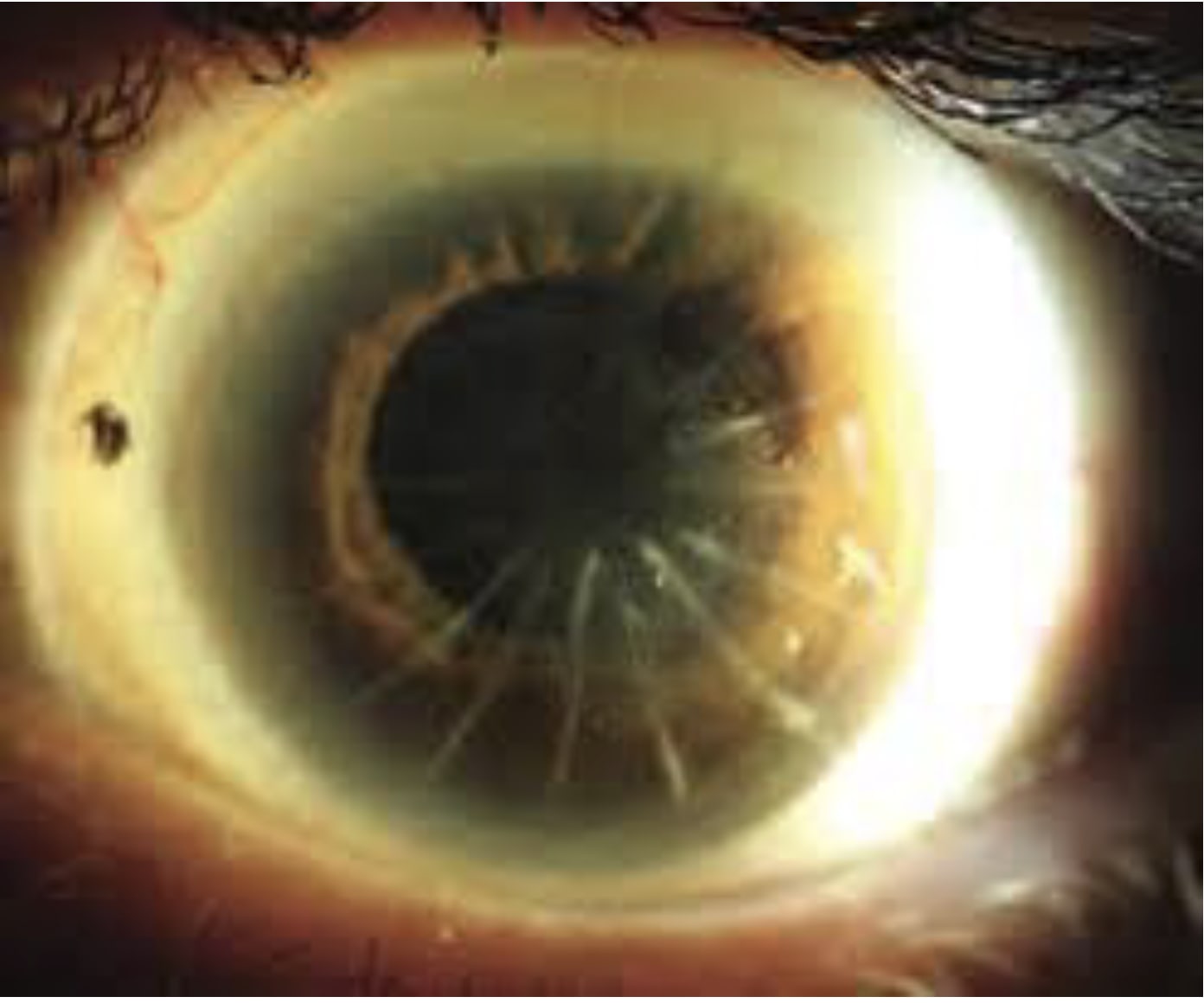
In the 15 states that enable optometrists to perform laser procedures, the most popular is yttrium aluminum garnet (YAG) laser capsulotomy. In recognizing this, Joe Munsell, OD, dedicated part of his 2025 Optometry’s Meeting lecture, “Optometric Laser Procedures: Pearls, Pitfalls, and How to Successfully Incorporate Into Your Practice,” to clinical pearls related to the procedure.
“When performing YAG caps, set yourself up for success,” he said.
Select the Ideal Patient
Dr. Munsell described the ideal YAG capsulotomy patient as someone who has no confounding factors, such as diabetic retinopathy or glaucoma. Additionally, he mentioned that although filtering blebs are not a contraindication to the procedure, ODs should exercise caution here, as the procedure can result in increased intraocular pressure (IOP), should the bleb dysfunction.
Wait at Least 3 Months
The optometrist should wait at least 3 months after cataract surgery before performing a YAG capsulotomy because this is typically the time it takes for the eyes to heal after their cataract surgery, pointed out Dr. Munsell. Further, he cautioned that performing the laser procedure too soon has resulted in cystoid macular edema, intraocular lens damage or placement shift, an IOP spike, retinal tears, and retinal detachments.
Consider a Focusing Lens
Dr. Munsell noted that although the OD can perform a YAG capsulotomy without a focusing lens, known as an Abraham lens, he recommended the optometrist use the magnifying lens to ensure laser accuracy and patient stability when first starting to perform this procedure.
Choose the Energy Setting/Technique
If the patient has a fibrous posterior capsular opacification, Dr. Munsell recommended setting the laser to 1.3 mJ to 2.5 mJ, noting that he’s achieved the most success from 1.7 mJ.
Additionally, Dr. Munsell suggested the space between the laser’s focal point and the lens’ posterior capsule be 125 μm to 500 μm, with his personal sweet spot being 250 μm.
Finally, Dr. Munsell recommended using the cruciate technique to open the posterior capsule, starting perpendicular. This technique enables the OD to prevent free-floating fragment formation in the vitreous, he explained. OM