Not all cases of persistent ocular discomfort are true dry eye. This was the message of the presentation, “Dry Eye Masqueraders: What To Do When Dry Eye Treatments Don’t Work,” given by Drs. Mila Ioussifova, Hardeep Kataria, and Ada Noh at the 2025 meeting of the American Academy of Optometry.
Ocular Allergy
One frequent culprit of ocular discomfort is ocular allergy, including seasonal allergy, vernal and atopic keratoconjunctivitis, and giant papillary conjunctivitis, the presenters pointed out. Such patients may present with itching, burning, and fluctuating vision that overlap with dry eye, yet underlying inflammation and meibomian gland changes suggest allergy as the driver. Interventions, such as antihistamine–mast cell stabilizers, allergen avoidance, and, in some cases, topical cyclosporine can provide relief, they explained.
Conjunctivochalasis
Conjunctivochalasis mimics dry eye by disrupting tear flow and causing irritation, according to the lecture. Symptoms include epiphora, fluctuating vision, and foreign-body sensation. While non-surgical options may help, advanced cases often require excision or tissue-shrinking procedures, the lecturers pointed out.
Corneal Dystrophies
Corneal pathologies, such as epithelial basement membrane dystrophy and Salzmann nodular degeneration, can produce dryness, glare, and fluctuating vision, according to the presentation. These may need specialized therapies, from lubrication, to keratectomy, the lecturers said.
Corneal Nerve Dysfunction
Another underrecognized masquerader of dry eye is corneal nerve dysfunction, characterized by underactive or overactive corneal nerves. It classically presents as a mismatch between signs and symptoms, pain without stain (corneal neuropathic pain), and stain without pain (neurotrophic keratopathy), according to the lecture. Corneal nerve dysfunction is best addressed through nerve-targeted treatments like amniotic membranes, biologic-derived drops and/or neuromodulators, said the lecturers.
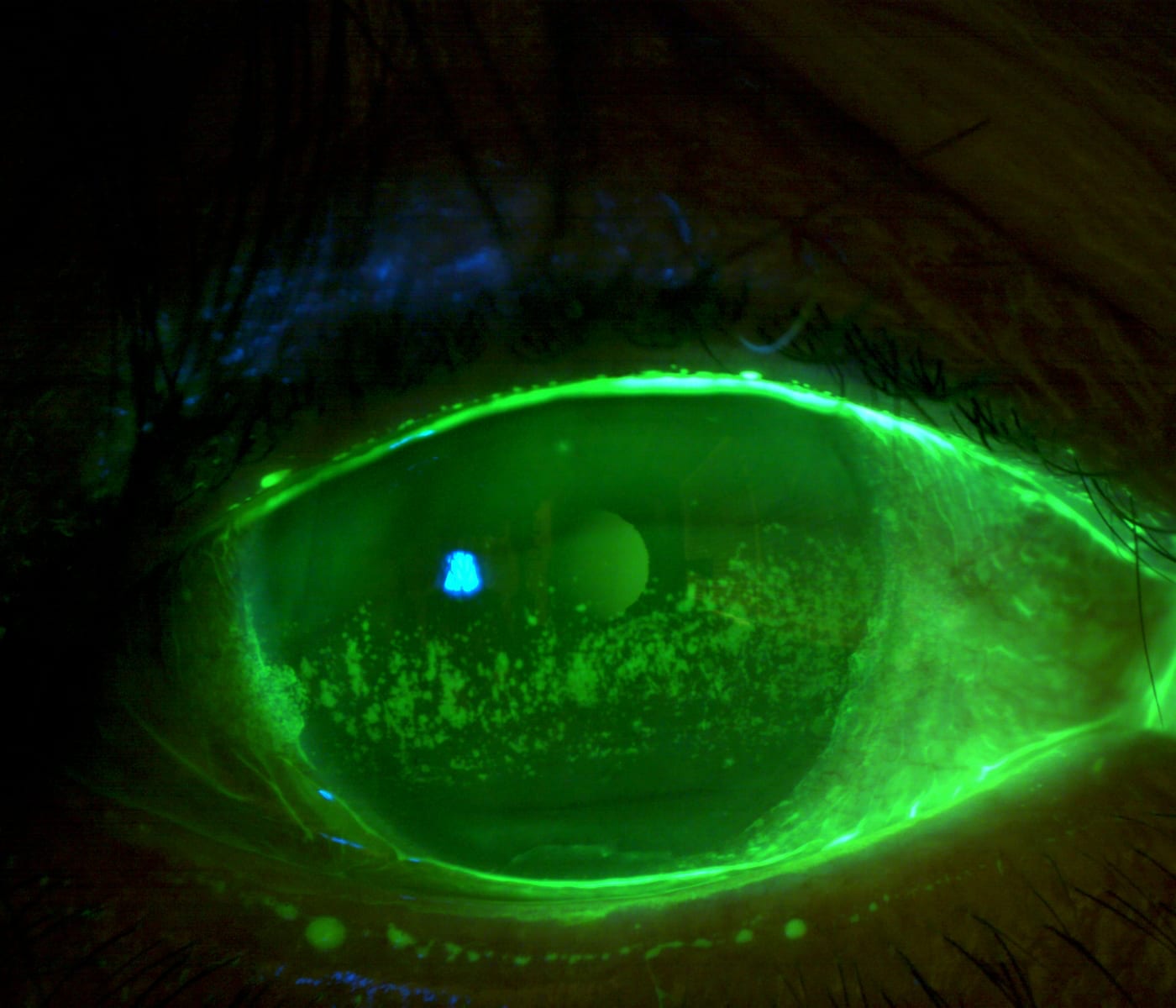
Friction Syndromes
Other sources of dry eye misdiagnosis include friction syndromes, mucin deficiencies, superior limbic keratoconjunctivitis, FK, mucus fishing syndrome, and post-glaucoma surgery. Staining both the conjunctiva and cornea provides a complete picture, the lecturers explained. Targeted therapies, such as mucin secretagogues, anti-inflammatories, or mucolytics, may prove successful in treating friction syndromes, they said.
Eye Anomalies
Types of eye anomalies, such as entropion, ectropion, and floppy eyelid syndrome, can also masquerade as dry eye. Eyelids may not close all the way, especially during sleep—this occurs in 61% of dry eye symptom patients, according to the lecture. Ointments, sleep masks, and eyelid tape may be possible treatments, but more severe cases may need surgical intervention, the lecturers noted.
The key takeaway: “When dry eye therapies fail, look beyond dry eye,” said Dr. Ioussifova. “Masquerading conditions often mimic the signs and symptoms of dry eye, and identifying these hidden culprits is the key to delivering true relief and improving patient satisfaction.” OM



